Program Year 8: July 1, 2025 - June 30, 2026
Frequently Asked Questions
What is BestHealth?
BestHealth is a comprehensive, voluntary health and wellbeing program provided by the Baptist Memorial Health Care Corporation (BMHCC) to give you the tools and support you need to live your healthiest life.
The BestHealth Wellbeing Program offers eligible Baptist employees the opportunity to earn up to $300 in rewards and avoid a $100/month tobacco surcharge on their medical insurance plan. Program participation is voluntary but encouraged, as it supports a healthier lifestyle and offers significant financial incentives. If your BlueCross BlueShield (BCBS) medical insurance begins on or after October 1, 2025, you do not need to complete a biometric screening and will not be charged the tobacco surcharge for 2026.
What services does BestHealth offer?
- An online Health Risk Assessment Questionnaire & Health.
- A BestHealth-approved biometric screening with a Primary Care Provider is completed once a program year, which is July 1st – June 30th.
- Wellbeing rewards up to $300 each program year for meeting health goals.
- A BestHealth-approved biometric screening.
- Wellbeing programs, classes, and 1-on-1 health coaching and care coordination to help you set and achieve your personal health goals.
Who is eligible to participate in the services BestHealth offers? A check mark indicates who is eligible to participate in each service offered.
To participate in the BestHealth program and earn rewards, you must be enrolled in the BlueCross BlueShield (BCBS) medical insurance plan through Baptist. Only employees enrolled in BCBS are eligible for rewards and tobacco surcharge waivers. Spouses and dependents with medical coverage may participate in select programs but are not eligible for rewards unless they are Baptist employees.
How do I become a member of BestHealth?
To become a member of BestHealth, you must first be eligible to participate. Eligibility requires that you are currently enrolled in the BMHCC health insurance plan; specifically enrolled in medical coverage. Once eligible, (normally 2 weeks after effective date of insurance) you will need to create an online account and complete an online health risk assessment questionnaire with inHealth wellbeing.
To create an online account with inHealth Wellbeing:
Download the inHealth: Wellbeing mobile app or visit the web portal at myhealth.inhealth4change.com.
First-time user?
- Click Create Account on the sign-in page.
- When prompted, enter the company ID: BMHCC.
- Complete all account information and accept the Terms of Service.
Tips:
- Password must be 8–15 characters with at least one number and one special character (! @ # $ % ^ & *).
- Use the last 6 digits of your SSN when prompted.
- If you do not have a physician, enter “NA.”
- Having trouble? Click here for detailed instructions.
Already registered?
- Log in using your credentials.
- Forgot your email? Contact BestHealth at BestHealth@bmhcc.org or call 901-227-2378.
- Forgot your password? Click “Forgot Password” to have a temporary password sent to the email address associated with your account.
Step 2: Complete Your Health Risk Assessment Questionnaire (HRAQ)
- Log in to the inHealth: Wellbeing app or portal at inhealth4change.com.
- Access the Screening page from the main menu.
- Tap the Take Survey button in the Health Risk Assessment Questionnaire box.
- Once you complete the questionnaire, you will be prompted to review the Consent Form. Enter your name exactly as it appears in your account and click, I Agree to confirm consent.
- When you are ready to submit your questionnaire, tap Submit Now.
What if I am unable to participate in BestHealth due to a limitation or disability?
If a health condition or disability prevents you from completing a biometric screening, tobacco test, or other program components, you may qualify for reasonable accommodation or alternative standards. Contact BestHealth at BestHealth@bmhcc.org or call 901-227-2378 (BEST) for assistance.
What is a BestHealth-approved biometric screening and what does it measure?
A BestHealth-approved biometric screening is a series of health tests performed by a Primary Care Provider to offer insight into your overall health. It includes measurements of height, weight, waist circumference, Body Mass Index (BMI), blood pressure, heart rate, blood glucose, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, and a tobacco or cotinine test (a biomarker for tobacco exposure).
Who is eligible to have a BestHealth-approved biometric screening completed by a Primary Care Provider?
Any employee and spouse enrolled in the Baptist BlueCross BlueShield (BCBS) medical insurance plan are eligible. BCBS covers a wellness visit and biometric screening each year. You do not have to wait 365 days between visits.
As an employee enrolled in BCBS medical coverage, am I required to be a BestHealth member and complete a biometric screening and tobacco test between July 1, 2025 – November 14, 2025?
Yes—if you want to avoid paying a $100/month tobacco surcharge for the 2026 benefits year. You must be a BestHealth member, complete the Health Risk Assessment Questionnaire, undergo a biometric screening, and test negative for tobacco/nicotine by November 14, 2025. This also qualifies you to earn up to $300 in rewards. Primary health insurance members are required to complete the biometric screening to avoid incurring a $100 monthly tobacco surcharge.
If I am a new employee, when do I need to complete the screening and tobacco test to avoid the surcharge for 2026?
- Hired before October 1, 2025: You must complete the HRAQ, biometric screening, and tobacco test between July 1 and November 14, 2025.
- Hired on or after October 1, 2025: You will not be charged the $100/month tobacco surcharge for the 2026 benefits year. You may still complete the screening (no tobacco test required) between January 1 and June 30, 2026 to earn up to $300 in rewards.
Can I complete only the tobacco/cotinine test to avoid the surcharge?
No. A tobacco/cotinine test alone is not accepted. You must complete both the tobacco/nicotine test and the full biometric screening by November 14, 2025.
Is my spouse required to complete a biometric screening or tobacco test?
No. Spouses are not subject to the $100/month tobacco surcharge and are not required to complete the screening or tobacco test.
How do I schedule a biometric screening with my Primary Care Provider?
- If using a Baptist Medical Group (BMG) Primary Care Provider: When scheduling your appointment and at your visit, inform them that you need to complete a BestHealth-approved biometric screening. BMG has the BestHealth-approved biometric screening form and will send electronically to BestHealth.
- If using a non-BMG Primary Care Provider: When scheduling your appointment and at your visit, inform them that you need to complete a BestHealth-approved biometric screening and that you will bring a BestHealth-approved biometric screening form with you to the appointment. The Primary Care Provider will fax the completed screening form to BestHealth, and a copy of the official tobacco results should be attached. The BestHealth-approved biometric screening form can be found in the inHealth Wellbeing portal at myhealth.inhealth4change.com or on the inHealth: Wellbeing mobile app, the BestHealth Sharepoint site, or email BestHealth at BestHealth@bmhcc.org to request a screening form. If you don’t have a Primary Care Provider and need assistance locating one, please email BestHealth at BestHealth@bmhcc.org or call 901-227-2378 (BEST).
Can I combine my wellness exam with the biometric screening?
Yes. Let your provider know you want both your annual wellness visit and BestHealth biometric screening during the same appointment. One free annual wellness exam is covered per calendar year (Jan 1–Dec 31).
Does Baptist pay for the screening?
Yes. For employees only. Any additional testing is your financial responsibility. Both employees and spouses are eligible for one free wellness visit per calendar year.
Can I go to my screening appointment while on the clock?
No. You must schedule your screening on personal time.
What must I and/or my spouse complete before going to the BestHealth-approved biometric screening?
- You must complete an online Health Risk Assessment Questionnaire located on the inHealth Wellbeing mobile app or web portal, and it must be completed each program year (July 1- June 30).
- For current BestHealth members, login to your inHealth Wellbeing account through the inHealth Wellbeing mobile app or web portal at inhealth4change.com. On the main page, click on the Health Risk Assessment Questionnaire, complete, and submit.
- If you’re not a current BestHealth member and meet the eligibility requirements, you must create an online account with inHealth Wellbeing through the inHealth Wellbeing mobile app or web portal at myhealth.inhealth4change.com (company code is BMHCC). Once the account is created, login, click on the Health Risk Assessment Questionnaire, complete the form, and submit.
What are the pre-screening instructions before going to my BestHealth-approved biometric screening?
- Fast at least 6 hours before your appointment for the most accurate.
- Take your medications as prescribed with water.
Can I use previous blood work?
Yes—if it was completed within the past 180 days and includes blood glucose, cholesterol, and triglycerides. The cotinine test must be current each program year.
How will I know if BestHealth received my screening results?
You’ll receive a confirmation email. You can also log in to the inHealth portal or app and check the Rewards section. A green check mark next to “Biometric Screening” means your results have been received.
How can I view my screening results?
Log in to the inHealth portal or app and click on Screening Results. You’ll see a comparison of your most recent and initial results.
What does BestHealth do with screening and assessment information?
This data helps you better understand your current health and risks. It’s also used to offer personalized wellbeing services like coaching, programs, and health classes.
What are the Wellbeing rewards?
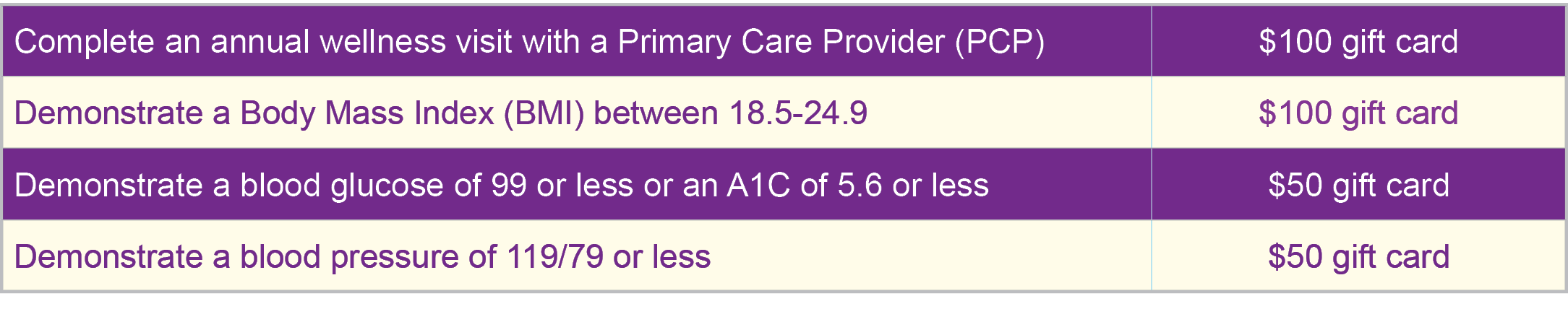
BestHealth is committed to creating a culture of support through a holistic approach to health. As a BestHealth member, you can earn up to $300 in wellbeing rewards each program year (July 1, 2025 – June 30, 2026) by completing a BestHealth-approved biometric screening and meeting designated health targets. Rewards are based on key outcomes from your screening and annual wellness visit with a Primary Care Provider.
How do I see if I earned any Wellbeing rewards from my BestHealth-approved biometric screening?
Log in to your inHealth Wellbeing account via the mobile app or web portal. Select Rewards from the menu. A green checkmark next to a category means you’ve earned that reward.
When will the Wellbeing rewards be available to redeem?
Rewards will be available after October 15, 2025, or two weeks after your biometric screening results have been received and processed by BestHealth. You must currently be enrolled on the Baptist BCBS medical insurance plan to redeem your rewards.
Will I receive an email notifying me that my Wellbeing rewards are available?
Yes. You will receive an email at the address associated with your inHealth account once your rewards are ready to be redeemed.
How do I redeem my Wellbeing rewards once they’re available?
Visit besthealth.awardco.com.
- First-time users: Use the employee ID number (on the back of your badge) as both your username and password. You’ll be prompted to reset your password.
- Returning users: If you’ve forgotten your credentials, contact Awardco at support@awardco.com
or 1-800-320-0893.
Once logged in, hover over “Spend Dollars” to view your reward redemption options.
If I didn’t meet reward thresholds for BMI, blood pressure, and/or blood glucose during my biometric screening, can I still earn those rewards later?
Yes. You have a few options:
- Participate in a complimentary program such as FLOURISH Lifestyle Management, Diabetes Education or Prevention, or one-on-one Health Coaching.
- Ask your Primary Care Provider to recheck your unearned values and submit an updated BestHealth-approved biometric screening form to BestHealth.
You’ll receive the reward(s) if you meet the required values. Screening forms are available via the inHealth portal, app, BestHealth SharePoint, or by request at BestHealth@bmhcc.org.
If I’m still employed but no longer enrolled in the BMHCC medical insurance, can I redeem my rewards?
No. You must be actively enrolled in Baptist’s BCBS medical coverage to redeem rewards.
If I’m no longer employed at Baptist, can I still redeem my rewards?
No. Employment at Baptist is required to access and redeem wellbeing rewards.
What programs are available for pregnant or postpartum employees to earn the BMI reward?
BestHealth provides targeted support for expecting and new mothers:
- Healthy Mom, Healthy Baby is an 8-week maternity education and support program designed to guide you through pregnancy and Topics include nutrition, childbirth, returning to work, and more.
- Eligibility: If you are currently pregnant or less than 6 months postpartum, you may enroll.
- Flourish Lifestyle Management
- Dietary Lifestyle Transformation
How do I avoid paying the $100/month tobacco surcharge for the 2026 benefits year?
All employees enrolled in the medical coverage of the Baptist BCBS health insurance plan (primary insurance holder only; not spouse or dependents) must:
- Become a member of BestHealth.
- Complete a BestHealth-approved biometric screening.
- Test negative for tobacco/nicotine with a Primary Care Provider.
These steps must be completed between July 1 and November 14, 2025 to avoid the $100/month tobacco surcharge for the 2026 benefits year.
Can I complete only a tobacco or cotinine test to avoid the surcharge?
No. A tobacco or cotinine test alone will not be accepted. You must complete a full BestHealth-approved biometric screening and test negative for tobacco/nicotine between July 1 and November 14, 2025.
How can I check if I tested negative for tobacco?
Log in to your inHealth Wellbeing account through the mobile app or at myhealth.inhealth4change.com.
- Go to Rewards on the menu.
- A green check mark next to Tobacco Free indicates that you’ve met the requirement and will not be charged the surcharge.
You may also contact BestHealth at BestHealth@bmhcc.org or 901-227-2378 (BEST) to confirm your status.
If I test positive or self-attest to tobacco use, can I still avoid the surcharge?
Yes. To have the $100/month surcharge waived for the full 2026 benefits year, you must:
- Enroll in and complete the 5-week virtual BestHealth Tobacco Cessation Course.
- The course must be completed between July 7 and November 17, 2025.
You can sign up at: https://form.jotform.com/BaptistBestHealth/fall-2025-tobacco- cessation-sign-up
What is the BestHealth Diabetes Management Program?
The BestHealth Diabetes Management Program will help you take an active role in managing your diabetes by working with our wellbeing specialists and care coordinators on your personalized care plan. Our approach focuses on improving your overall health and wellbeing while helping you learn how to manage diabetes better. BestHealth wellbeing specialists and care coordinators, in partnership with your healthcare provider, will aid you in setting and achieving goals. Participants meeting all requirements of the program receive 100% coverage of approved medications and supplies, including medically necessary needles, syringes, lancets, test strips, and glucometers to treat diabetes.
Who is eligible to participate in the BestHealth Diabetes Management Program?
All BMHCC Employee Health Plan enrolled employees, spouses, and dependents with a diagnosis of type 1 diabetes, type 2 diabetes, gestational diabetes, insulin resistance, or prediabetes who have completed a BestHealth Health Risk Assessment (HRA) and Biometric Screening within the current program year are eligible to enroll in the program.
What is the benefit of participating in the BestHealth Diabetes Management Program?
Participants enrolled in the BestHealth Diabetes Management Program will receive 100% coverage of approved diabetic medications and supplies, including medically necessary needles, syringes, lancets, test strips, and glucometers.
Health Coaching: Enrolled participants will be assigned a wellbeing specialist or care coordinator to assist with improved management of their disease and overall wellbeing. Wellbeing specialists or care coordinators will work with enrolled participants by phone, email, or in-person to establish personalized diabetes and health management goals and monitor results.
How do I enroll in the BestHealth Diabetes Management Program?
- Complete a BestHealth Screening.
- Adult and dependent members ages 18 and older must enroll in BestHealth by completing a BestHealth biometric Call (901) 227-2378 to learn how to complete the screening process if you have not completed one. *Dependents under the age of 18 are not eligible to screen therefore must submit a physical examination from their physician.
- Have your provider complete and send the Provider Verification of Diagnosis Form to BestHealth.
- Review, sign, and submit the Enrollment Form to BestHealth.
Upon receipt of a completed Enrollment Form, a BestHealth representative will contact you to complete the enrollment process.
To enroll in the program, complete the BestHealth Diabetes Management Program Enrollment Packet and submit to BestHealth via email (besthealth@bmhcc.org) or fax (901) 227-2377. The provider verification of diagnosis form must be faxed by your provider.
Once I complete the enrollment process, when will my $0 copay take effect?
After completing all the required steps of the enrollment process, your benefit will go into effect on the 1st of the following month if you have had your initial session with your Wellbeing Specialist or Care Coordinator by the 25th of the month prior. For example, if you finish the enrollment process on September 14th, your benefit will go live on October 1st.
I have not completed a BestHealth HRA and Biometric Screening. Can I still participate in the BestHealth Diabetes Management Program?
The BestHealth HRA and Biometric Screening must be completed during the current BestHealth program year to be eligible for the program. If you have not done so, call BestHealth at (901) 227-2378 for more information on how you can complete the BestHealth HRA and Biometric Screening and enroll in the BestHealth Diabetes Management Program.
What are the requirements to remain enrolled in the BestHealth Diabetes Management Program and maintain the pharmacy benefit?
In order to remain enrolled in the program and maintain the pharmacy benefit, participants must meet the following minimum requirements:
- Pharmacist will review the current medication regimen and discuss any recommended changes with the member and/or provider.
- Meet with a BestHealth wellbeing specialist or care coordinator at least every 3 months via in-person visit or telephone. Wellbeing specialists, care coordinators, and/or medical providers will determine the required contact frequency using clinical judgment based on the severity and individual needs of the participant.
- Provide blood sugar log results at each coaching session. Participants not required by the medical provider to perform home blood glucose monitoring must annually submit an attestation from the medical provider indicating that home testing is not required.
- Participants with a BMI of 25 or greater must complete the Flourish Lifestyle Management program annually within 6 months of the start of the current benefit plan year or enrollment in the BestHealth Diabetes Management Program.
- Complete an annual wellness exam with a primary care provider.
- Documentation of biannual HbA1c by the wellbeing specialists or care coordinators from the medical record or submitted via attestation form by participants. *Additional requirements may be needed based on A1c.
- Complete annual diabetes care requirements, including blood pressure, cholesterol, HbA1c, microalbumin, diabetes eye and foot exams, and flu vaccine as recommended by the medical provider.
*Anyone with an A1c of 8 or above must complete the Diabetes Educational modules annually.
How do I access the BestHealth Diabetes Management Program pharmacy benefit?
Once enrolled in the program, participants must present a prescription to purchase diabetes medications and supplies. While we encourage the use of a designated BMHCC pharmacy or BMHCC mail order for convenience and coordination, it is not required.
What medications and supplies are covered at no cost to enrolled participants?
Provider-prescribed medications and supplies, including medically necessary needles, syringes, lancets, test strips, and glucometers to treat diabetes, that are included on the BMHCC Employee Health Plan Formulary will be covered at no cost to enrolled participants.
Members must present a prescription to purchase diabetic medications and supplies at no cost. While participants are encouraged to use a designated BMHCC pharmacy, this is not mandatory, except in cases where state-specific limitations apply.
What happens if I am not compliant with the requirements of the program?
Enrollment in the BestHealth Diabetes Management Program benefit will cease on the date a wellbeing specialist or care coordinator determines that the participant is no longer compliant with the requirements of the program. At that time, all prescriptions for diabetes supplies and medications will be subject to the standard copays and deductibles of the pharmacy plan elected during BMHCC Health Plan enrollment.
Disenrolled participants continue to be eligible to participate in BestHealth health coaching, care management, and wellbeing programming.
Can I re-enroll in the program once I have been disenrolled?
Participants who have been disenrolled from the BestHealth Diabetes Management Program are not eligible for the BESTHealth Diabetes Management Program pharmacy benefit until the start of the next benefit plan year.
Whom should I contact with questions?
For questions regarding the Diabetes Management Wellbeing program, you can email BestHealth@bmhcc.org.
What phone number can I call for further assistance?
(901) 227-2378
What is the BestHealth Care Coordination Program?
Baptist Memorial Health Care highly values the health and well-being of our employees. Through the BestHealth employee Care Coordination program, employees and spouses on the health care plan can receive additional care coordination support from a registered nurse at no additional cost to you. These nurse care managers provide health promotion and guidance on appropriate care options, lessening the money you will spend on healthcare and improving the quality of care you receive.
What does a BestHealth nurse care coordinator do?
A BestHealth nurse care coordinator provides seamless management of care for all levels of healthcare- preventative, primary, and specialty care. These nursing care coordinators work to keep your doctor informed, help you create a well-being vision, create meaningful and personalized health goals, and provide you with additional educational resources and materials. Our goal is to give you tools and information to empower you to choose how you independently manage your health and well-being through disease prevention and management of long-term medical conditions.
What is involved in the BestHealth Care Coordination program?
Typically, you engage with the nurse telephonically for 30-60 minutes once or twice a month, where you will work together on two or three meaningful goals to your specific health needs. For example, some patients want help understanding or affording their
medications, finding providers and community services, or working on lifestyle changes like diet, increasing activity, or quitting smoking.
Is the BestHealth Care Coordination program confidential?
Your personal health information is protected under HIPAA and is only available to nurse care coordinators and your care team. The nurse care coordinator will never share your protected health information without expressing your permission with those outside of your care team. Electronic communication is utilized with written consent. We utilize HIPAA guidelines when communicating with practices and providers.
What are the benefits of working with a BestHealth Nurse Care Coordinator?
A Nurse care coordinator is a personalized extension of your care team, acting as a guide and advocate to help keep you healthy and make life easier.
The nurse can manage care for things such as:
- Management of a chronic condition (e.g., asthma, coronary artery disease (CAD) & hypertension, chronic obstructive pulmonary disease (COPD), heart failure, diabetes).
- Management of multiple significant conditions.
- Care management and connecting with resources for food, transportation, housing, and finances.
- Transitions of care after surgery or hospital visit.
- Follow-up after a visit to the Emergency Department.
- Medication review.
How do I opt for the BestHealth Care Coordination program?
You automatically have access to Nurse Care Coordinator outreach as part of the Baptist health plan.
Contact BestHealth to enroll today – call (901) 227-2378 (BEST)
Achieve Your BEST Health!
Take small steps toward reviving your overall wellbeing! Our programs will help identify personal challenges, set goals, and encourage healthier lifestyle behaviors.
Wellbeing specialists and care coordinators are ready to support your wellbeing journey!
To learn more about the BestHealth Wellbeing Program and how you can earn exciting rewards on your journey to better health view our program page: